
Recent approvals of viral gene therapies have reached records in cost of dose, up to the most recent approval of HEMGENIX priced at 3.5M$ per dose. In this article we look at how process development, cost modelling and process intensification can help drive cost of dose down.
Gene therapy is a fast-growing sector in the life sciences industry, and there are countless reasons to be enthusiastic about it. The fact that we can use specific gene-modifying technology to amend genetic disorders and provide patients with such impactful treatment is amazing. We have seen an increase in drugs approved over 2021 and 2022, and there are several others pending approval in 2023 - 2024. When we look at the clinical trial pipeline, one can only wonder whether we could reach 10 to 25 approvals per year by 2025. The idea of having all these approved potentially curative therapies on the market is certainly exciting. However, the question of the accessibility to these drugs by the wider population is still unanswered. Indeed, the last 4 drugs approved by health authorities range between 2.5 and 3.5 million dollars per dose (respectively Roctavian®, Zynteglo ®, Skysona ® and Hemgenix ® approved by the FDA just end of 2022). In some cases, regulatory agencies have even withdrawn approval as a direct result of the pricing such as the case of Skysona in EU, withdrawn at the request of the manufacturer for commercial reasons, or Zynteglo who had to be pulled out of Germany due to the government officials refusing to pay the listed price.
If we compare the cost per dose of these approved drugs with a lifetime of treatment, the cost is usually justified. In a recent article, the example of the recent Hemgenix® approval was taken. The $3.5 million single dose treatment would replace a lifetime treatment up to $20 million for Hemophilia B patients. However, in the healthcare system we live in, these single dose prices are not compatible with giving the wider population access to all these potentially curative therapies almost at the same time. This is even more true when we think of ultra-rare diseases, as the amount of research and development necessary is usually comparable but the patient population, being much smaller, leads to a much lower drive for return. Something has to change.
There are many angles from which we could tackle this. Manufacturers could be pressured to decrease the prices. But why would they do that? Of course, these drugs are the fruits of years of R&D, and the investment in R&D is clearly a large part of the cost, as it includes accounting for the risks associated with developing a drug that will take a lot of effort to reach the market and might not get approved in the end. A recent study published in 2021 estimated that “R&D costs per new medicine (accounting for the cost of failure) ranged from $944m to $2,826m (adjusted to 2019 prices)”. The current cost of manufacture is far harder to define. Even if the manufacturing platforms were identical, just differences in the dose required could mean more than a 1000-fold difference. While this cost is smaller than the R&D costs, it still has an impact and this is a part of the cost that we, as industrialists, can help to reduce. If successful this helps the manufacturer’s lower costs, while still being profitable.
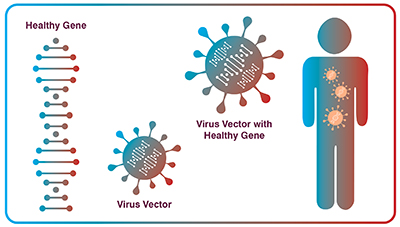
When we look at that last part, the high cost of manufacturing and the direct cost of a dose is a combination of many factors, but I believe there are two main ones. The first one is the actual quantity of product that is going into the patient compared to the total quantity of material produced. Indeed, some case studies outline that for a phase 3 clinical trial, only 2% of the product that is manufactured actually goes into the patient (Blue, 2022, 16:56). This percentage might increase slightly once the product moves into routine production, but there is still a large part of the manufactured product that is used for analytical testing, comparability studies, assay controls, stability testing, device losses… the list of points where losses occur goes on. Optimizing the methods around analytics, stability testing, and material requirements overall will help increase the quantity of product produced and that can be administered to the patient. This ultimately decreases cost per dose. The second one is that we are manufacturing these therapies, these viral vectors, with technologies that have mostly been developed for the mAb and recombinant protein industry. They are ok and have enabled more and more approved products to reach the market. But they could be better if specially developed for viral vectors. There is a major lack of process maturity and adapted technologies. This is an area where solution providers will have a major role to play.

Let’s keep focus on that last point. Solution and technology providers are constantly looking to drive innovation in the way we manufacture products, and drug developers are constantly seeking higher performing processes. Closing the gap on the technologies for viral vector production can only be achieved through close collaboration between drug manufacturers and technology providers. This is the only way we can maximize the chances of developing the right product that the industry needs, in the shortest time. By using more adapted technologies specially developed for these specific products, we will be able to increase the total productivities, increase the recovery and ultimately leading to a decrease in the manufacturing cost per dose. Keeping close contact with regulatory experts through this process will also help making sure the improved technologies will not raise more concerns that they bring solutions.
When we look at the manufacturing process for a viral vector (e.g. adeno-associated virus or AAV, lentivirus or LV) the process can usually be broken into two parts: the upstream process (USP) and the downstream process (DSP). USP productivity can be optimized through bioprocess development/optimization, cell line optimization, plasmids and transfection reagent optimization, and in some cases the use of stable cell lines. To increase the DSP yield, the main levers are process optimization and better recovery at every step of the process. In the case of AAV manufacturing for example, DSP recovery is often around 25 – 30%, with a few achieving up to 40%. Therefore, in a worst-case scenario (25% yield), all the improvements we could think of such as better affinity ligands, innovative solutions to better purify these viral vectors, we can perhaps expect to improve the yield to 80% delivering a 3X yield improvement, and a probable decrease in cost per dose between 1.5 and 2X.
Most experts in this area align on the fact that we need to improve the yields at a factor between 10X and 100X in order to decrease the cost of these therapies significantly to facilitate their access and make them economically viable. So, the question is: how do we go from a 3X improvement to something that is closer to a 100X increase in yield? To do this we need to work on the USP. This includes the use of better plasmids and transfection reagents, stable producer cell lines, USP intensification (e.g. engineering cell lines to excrete AAV for example to make processing easier), improving the AAV full:empty ratio out of the cell and the infectious titer among others. USP optimization is the real cost lever that will help making these therapies more accessible.
What are the direct benefits of increased USP productivity? First, it means more doses per batch. This means more patients treated and thus a reduced direct cost per dose. Secondly, it means fewer batches are required to manufacture the target quantity of doses. This means less starting material, less labor and operational expense (OPEX) in general. Alternatively, it could mean same number of batches but enable a reduction of the bioreactor size required. This means, fewer skids, a reduction in consumables cost, and capital expenditure (CAPEX) investment and a smaller manufacturing footprint.
Many development scientists are focused on the day-to-day challenges and may not naturally look forwards to the future challenge of full-scale manufacture. But the fact remains that the molecule in development will need to be scaled up at some point to deliver a product to the market. We often encounter inefficient, unoptimized, poorly scalable and poorly manufacturable processes as a result. Hindsight will always highlight the importance of developing a process to manufacture a therapeutic molecule, such as a viral vector, with the final scale in mind. When this knowledge is available before development commences, this allows for the right choices in terms of technology to be made as early as possible in the drug development journey. Of course, one could argue that there are process changes that are allowed between Clinical phase 1 and 2 for example. But starting the clinical journey with the process that will be the closest to the final manufacturing sequence ensures process robustness with enhanced knowledge and a more reliable Chemistry, Manufacturing and Control (CMC) package. By starting with a process that is close to the final full-scale process, drug developers enter the clinic with substantial volume of historical data showing process consistency and reproducibility. To generate the most cost-efficient process, one should not only screen, test and choose the right technology available, but every step needs to be optimized.
Several published examples have shown how taking some time to screen reagents such as cell culture media or even transfection reagents in the case of a transient process can have a major impact on viral vector yield and therefore overall cost. Some companies have also been looking at ways to improve cell line productivity, either through cell line engineering and/or stable cell line establishment, others have been looking at innovative ways to improve productivity. Some recent studies have shown that by improving the USP productivity by 50%, the USP manufacturing costs would decrease by 33%.
Tools such as cost modelling can also help understand the impact on the cost of batch or dose of specific process optimizations, or even just pinpoint the main cost drivers of the process. This can help process developers tackle the right parameters to further focus optimization efforts in a more efficient way.
Whatever the process development strategy or process optimization we choose to improve USP productivity, it is highly likely this will be accompanied by an increase in total process and product related impurities and contaminants. This increase will likely have an impact on the DSP: An extra purification step might be required; the size of chromatography columns or filters might need to be increased. It is therefore important to constantly balance the yield improvement on the USP side with the extra cost required on the DSP side to ensure the cost improvement is still valid.
Another strategy that can help optimizing the cost of dose is what we call process intensification (PI). Process intensification looks at minimizing the sources of waste, called Muda by lean process practitioners. Waste is usually attributed to one of 7 different categories: Transportation, Inventory, Motion, Waiting, Over processing, Overproduction and Defects. Some business drivers for process intensification are cost of production, footprint reduction, manufacturing flexibility, time to market, facility use, scalability, ease of use… Process intensification has recently been used during the ChAdOx-1 chimpanzee adenovirus‐vectored SARS‐CoV‐2 vaccine development. In this paper, Joe et al. illustrate two examples of process intensification that have a direct effect on the cost without affecting product quality. The first example is the optimization of the upstream process with a lower multiplicity of infection (MOI), leading to a reduced virus seed (1 order of magnitude) keeping the same productivity, same critical quality attributes (CQAs) and same production time. The second example relies on the downstream process, where the team have proven that the pre-established process contained an unnecessary step for this particular virus purification. Thus, by removing this step before chromatography, the process was shortened while keeping similar CQAs (within specifications) and similar yield.
While the industry is moving towards the application of scientific and technical platforms to decrease time to market and costs as outlined above, it is essential that we keep in mind the importance of combining it with process intensification. As outlined in the SARS-CoV-2 example, for every new molecule developed, the platform should be reassessed to make sure it is as cost efficient as possible.
So, can we decrease the cost of dose of gene therapies? I believe the answer is yes. It will however require a combined effort of:
- The technology providers and developers to find levers to increase upstream productivity by 10 to 100 times through cell line engineering, capsid engineering, etc.
- The technology providers and developers to develop new manufacturing and characterization tools to make the processes more efficient;
- The broadening of process intensification and process optimization from the early stages of the drug development.
Scientists developing processes in research need to start thinking manufacturability from the very early stages, leveraging suitable platforms to avoid slowing the development of suitable processes.
- The health authorities, governments and manufacturers to rethink the way a treatment is invoiced to the social security and patients;
Gene therapies for ultra-rare diseases will never be commercially viable unless we drive these costs down. There is a need of real innovation to help shifting the paradigm of the cost of dose.
References:
[1] N. Pagliarulo, “Bluebird, winding down in Europe, withdraws another rare disease gene therapy,” BioPharma Dive, Oct. 21, 2022. Accessed: Jan. 03, 2023. [Online]. Available: https://www.biopharmadive.com/news/bluebird-withdraw-gene-therapy-europe-skysona/608666/
[2] A. Chakraverty, “Bluebird Bio Withdrawal Raises Gene Therapy Doubts in Europe,” Labiotech.eu, May 04, 2021. https://www.labiotech.eu/trends-news/bluebird-bio-gene-therapy-zynteglo/ (accessed Jan. 03, 2023).
[3] J. Cohen, “Despite Eye-Popping $3.5 Million Price Tag For Gene Therapy Hemgenix, Budget Impact For Most Payers Will Be Relatively Small,” Forbes, Dec. 02, 2022. Accessed: Jan. 03, 2023. [Online]. Available: https://www.forbes.com/sites/joshuacohen/2022/12/02/despite-eye-popping-35-million-price-tag-for-gene-therapy-hemgenix-budget-impact-for-most-payers-will-be-relatively-small/
[4] “The Era of One-Shot, Multimillion-Dollar Genetic Cures Is Here | WIRED.” https://www.wired.com/story/the-era-of-one-shot-multi-million-dollar-genetic-cures-is-here/ (accessed Jan. 03, 2023).
[5] S. Simoens and I. Huys, “R&D Costs of New Medicines: A Landscape Analysis,” Frontiers in Medicine, vol. 8, 2021, Accessed: Jan. 09, 2023. [Online]. Available: https://www.frontiersin.org/articles/10.3389/fmed.2021.760762
[6] C. Blue and J. Wilkinson, “Material Requirements to Support Gene Therapy Development,” BrightTALK, May 19, 2022. [Online]. Available: https://www.brighttalk.com/webcast/10519/523569
[7] S. A. Pezoa, A. Pennybaker, R. Alfano, and N. Hazi, “Chemically Defined Upstream and Downstream Lentivirus Production for High T Cell Transduction,” Sptember 2022.
[8] D. Mainwaring, A. Joshi, J. Coronel, and C. Niehus, “Transfer and scale-up from 10 L BioBLU®️ to AllegroTM STR 50 and STR 200 Bioreactors,” Cell and Gene Therapy Insights, vol. 7, pp. 1347–1362, Sep. 2021, doi: 10.18609/cgti.2021.178.
[9] A. Vervoort, K. Sutherland, J. de Jong, and J.-S. Diallo, “Bioprocess Modelling of Upstream Viral Vector Production Enhancement,” Edimbourg, Oct. 2022.
[10] E. Cameau, A. Pedregal, and C. Glover, “Cost modelling comparison of adherent multi-trays with suspension and fixed-bed bioreactors for the manufacturing of gene therapy products,” Cell and Gene Therapy Insights, vol. 5, pp. 1663–1674, Nov. 2019, doi: 10.18609/cgti.2019.175.
[11] S. Sitter, Q. Chen, and I. E. Grossmann, “An overview of process intensification methods,” Current Opinion in Chemical Engineering, vol. 25, pp. 87–94, Sep. 2019, doi: https://doi.org/10.1016/j.coche.2018.12.006.
[12] C. C. D. Joe et al., “Manufacturing a chimpanzee adenovirus-vectored SARS-CoV-2 vaccine to meet global needs,” Biotechnology and Bioengineering, vol. 119, no. 1, pp. 48–58, 2022, doi: 10.1002/bit.27945.
[13] K. Doxzen, “Gene therapies could change millions of lives - so how will we pay for them?,” World Economic Forum, Sep. 03, 2021. Accessed: Jan. 11, 2023. [Online]. Available: https://www.weforum.org/agenda/2021/09/gene-therapies-rare-diseases-payment-affoardable-drugs-medicine/
[14] “public-statement-skysona-withdrawal-marketing-authorisation-european-union_.pdf.” Accessed: Dec. 20, 2022. [Online]. Available: https://www.ema.europa.eu/en/documents/public-statement/public-statement-skysona-withdrawal-marketing-authorisation-european-union_.pdf